Cerebral Palsy Integrated Pathway (CPIP) – Hip Surveillance
Hip Dislocation in Cerebral Palsy
Cerebral Palsy is the most common form of neuro-disability amongst children in the UK, affecting 0.1% - 0.4% of live births. The initial brain injury causes abnormalities in muscle tone which can cause a number of musculoskeletal problems as the child grows.
One of the most common orthopaedic manifestations of Cerebral Palsy due to muscle spasticity is hip dislocation (the ball working its way out of the socket over time). The risk of hip dislocation increases with the severity of the condition, being much more common in wheelchair-bound children. These hip dislocations sometimes can only be picked up on an x-ray.


CPUP – The Start of Hip Surveillance
In Sweden in 2004, they began a programme of hip surveillance in children with Cerebral Palsy called CPUP. This system involved regular examinations from a physiotherapist, and x-rays of the hips taken at set intervals based on the severity of the condition.
This surveillance allowed them to reduce the hip dislocation rate from 11% to less than 1% with no unrecognised hip dislocations. It also allowed a reduction in the overall surgery rate from 40% to 15% with a shift towards smaller soft tissue operations. As it was so effective in Sweden, the work has spread to other countries in an attempt to improve the care for children throughout the world with Cerebral Palsy.
CPIPS – Cerebral Palsy Integrated Pathway Scotland
In 2014, all of the Healthcare Trusts in Scotland worked together to implement the Swedish model of CPUP. They have been running this system with very positive results and excellent feedback from staff and families taking part in the programme.
After the success in Scotland, they have offered the chance for other UK healthcare providers to join the programme. Nottinghamshire Health Care Trusts will be adopting the CPIP programme from April 2018.
What does this mean for my Child?
Once your child has been given a diagnosis of Cerebral Palsy, a referral will be made to the CPIP programme. You will meet with a community physiotherapist who will explain the system and ask for your consent to enrol your child in the programme. If you agree to join the CPIP system then your GP and paediatrician will be informed.
The physiotherapists will see your child every 6 months until the age of 6 years, and then once a year until they are 16 years old. At each visit they will perform the exact same examination and record the results on the CPIP database. This will act as an early warning system to tell us if any of the muscles are getting too tight.
Your physiotherapists will also refer your child for x-rays of their hips when necessary. The more severely affected your child is with Cerebral Palsy the more regular the x-rays will be. The results of these x-rays will also be entered onto the CPIP database.
The Traffic Light System
CPIP works on a traffic light system. From the 20 years of data from Sweden, standard ranges have been established for all of the measurements taken in the CPIP assessment. As soon as your child’s measurement is inputted into the database, it will immediately be labelled as green, amber or red.

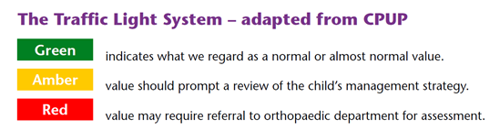
If all of the scores are green then everything is progressing without concern. No changes will be made to our child’s care
If there is a new amber or red value, this indicates that there is an early problem. Your child’s physiotherapist will work to try to stretch out any tight muscles and will seek advice from the paediatric and orthopaedic doctors as needed.
What are the Benefits of CPIP?
The CPIP programme is an early warning system which means that your child will be regularly reviewed. Muscle contractures (when the muscle gets so stiff it cannot fully stretch out) are responsible for a lot of the complications in Cerebral Palsy. If we identify these problems early, physiotherapy, splints and medicines to help reduce muscle tone can potentially avoid an operation.
We cannot totally eliminate the need for operations in children with Cerebral Palsy. We know from the work in Sweden, that surveillance and early intervention does reduce the number of children who need operations and that these operations tend to be smaller. This system gives your child the best chance of avoiding an operation, and makes it less likely that a major operation will be required if early measures fail.
What do I do if I have Any Questions?
If you have any questions or concerns regarding the CPIP programme, the best person to ask is your physiotherapist. If there is a question that they are unable to answer then they will be able to contact a paediatrician or orthopaedic surgeon who can answer your query.
